Knee Pain Causes and Remedies
KNEE PAIN
Causes & Remedies

Causes in Young Children and Adolescents
Bursitis. Osgood-Schlatter Disease
Runner’s Knee. Jumper’s Knee
Knock knees Bow Legs
Adults and Elderly
House Maids Knee (Bursitis). Osteoarthritis
Chondromalacia (Cartilage Erosion) Osteoporosis
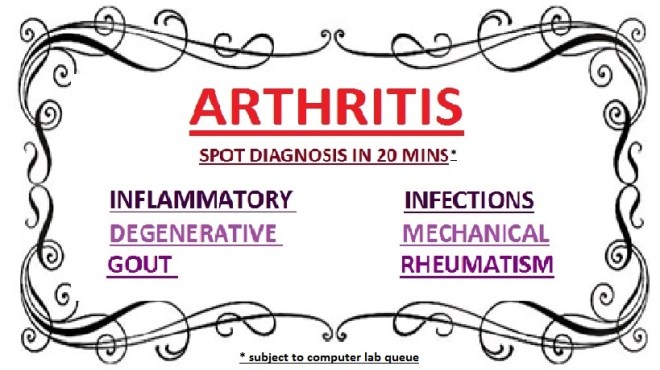
Gout, Septic Arthritis Rheumatic diseases
All ages
Vitamin D deficiency Vitamin C deficiency
Rheumatoid Arthritis. Ligament Injuries.
Topic Overview
Most people have had a minor knee problem at one time or another. Most of the time our body movements do not cause problems, but it’s not surprising that symptoms develop from everyday wear and tear, overuse, or injury. Knee problems and injuries most often occur during sports or recreational activities, work-related tasks, or home projects.
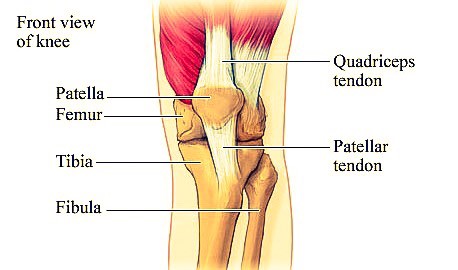
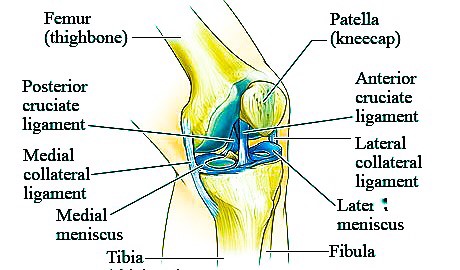
The knee is the largest joint in the body. The upper and lower bones of the knee are separated by two discs (menisci). The upper leg bone (femur) and the lower leg bones (tibia and fibula) are connected by ligaments, tendons, and muscles. The surface of the bones inside the knee joint is covered by articular cartilage, which absorbs shock and provides a smooth, gliding surface for joint movement. See a picture of the structures of the knee above.
Overview of knee pain
People have had a minor knee problem at one time or another. Most of the time our body activities do not cause problems, but it’s not surprising that symptoms develop from everyday wear and tear, overuse, or injury. Knee problems and injuries most often occur during sports or recreational activities, work-related or home activities.
The knee is the largest joint in the body. The upper and lower bones of the knee are separated by two discs (meniscus). The upper leg bone (femur) and the lower leg bones (tibia and fibula) are connected by ligaments, tendons, and muscles. The surface of the bones inside the knee joint is covered by articular cartilage, which absorbs shock and provides a smooth, gliding surface for joint movement. See the above picture of the anatomy of the knee.
Injuries are the commonest cause-
Sprains, Strains, or other injuries to the ligaments and tendons that connect and support the kneecap.
Meniscal tear in the rubbery cushions of the knee joint.
Ligament tears, such as the anterior cruciate ligament (ACL). The medial collateral ligament (MCL) is the most commonly injured ligament of the knee.
Fractures of the kneecap (Patella), lower portion of the femur, or upper part of the tibia or fibula. These are most commonly caused by abnormal force, directly falling on the knee, a severe twisting and/or bending motion, or when the knee forcefully hits an object while walking.
Kneecap dislocation.
Pieces of bone or tissue (loose bodies) from a fracture or dislocation that may get trapped in the joint and restrict movement. It could lock the knee
Knee joint Dislocation. This is a rare injury that requires violent force. It is a serious injury and requires emergency medical attention.
Knee Inflammation can be due to rheumatism, gout (elevated serum uric acid) or intra-articular infections (septic arthritis) especially in children.
Chronic use/overuse injuries and conditions like osteoarthritis (wearing down of the cartilage due to use and ageing), patellar syndromes, patellar tendinitis and bursitis.
Causes in children include Osgood Schlatter’s disease
Risk Factors: Altered Bio-mechanics, Overweight, Overuse during repetitive motions
Symptom Check List. – Consult your Doctor – When
• The hurt limb or joint looks odd, is an abnormal shape.
• The skin over the site of an injury has an open wound.
• You have signs of nerve or blood vessel injury, such as:
• Numbness, tingling, or a pins-and-needles feeling.
• Skin that is pale, white, or blue, or feels colder than the skin on the uninjured limb.
• Not being able to move the limb normally because of weakness and/or pain.
• You cannot put weight on or straighten an injured limb.
• Joint wobbles or feels unstable (gives way).
• You have severe pain.
• You have a swelling appearing within 10-20 minutes of the injury.
• Swelling and pain do not improve after a days of home treatment.
• You have signs of infection (fever & body ache, increased pain, swelling, warmth, and redness) after an injury.
Home Remedy
- Rest and protect an injured area. When resting, place a small pillow under your knee.
- Ice will reduce pain and swelling. Apply cold/ice packs immediately to prevent or reduce swelling for 10 to 30 minutes, 4 or more times a day.
- For the first 24- 36 hours after an injury, avoid things that might increase swelling, such as hot showers, hot packs, or alcoholic drinks.
- After 36 to 48 hours, if swelling is gone, apply moist Heat or alternate Heat/Cold and begin gentle exercises to help restore and maintain function.
- Compression, or wrapping the injured area with an elastic bandage using mild to moderate tension (such as an Tube-grip Stockings), will help decrease swelling
- Tight Bandage can cause more swelling below the affected area. Loosen it if required. Don’t expect the bandage to protect or stabilize a knee injury. Splints and
- Braces can be used.
- Talk to your doctor if you think you need further advice.
- Elevate the injured area on pillows while applying ice and anytime you are sitting or lying down. Try to keep the area at or above the level of your heart to help reduce swelling.
- Use a cane or crutch in the hand opposite your painful knee.
- Use two crutches, keeping weight off the leg with the sore knee. You can get canes or crutches from nearby pharmacies. Crutches are recommended if a cane causes you to walk with a limp.
- Gently rub the area to relieve pain and encourage blood flow. Do not massage.
Try the following exercises if you can to maintain function: Hamstring stretch, Knee-to-chest exercises - Avoid high-impact exercises such as running, skiing, snowboarding, or playing tennis, until your knee is without symptoms.
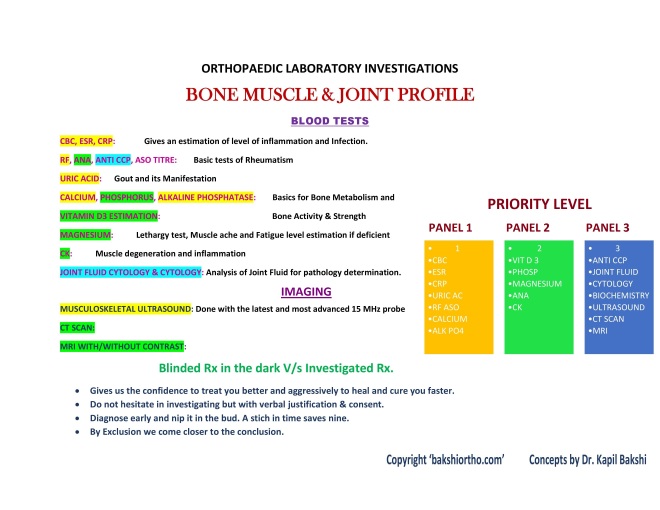
Investigations:
Radiological tests include X-ray, C.T and MRI.
Blood Tests include bone profile (CBC – complete blood count with ESR, RA test, CRP, Serum Uric Acid, Calcium, Phosphorus and Alkaline phosphatase).
SMOKING slows healing because it decreases blood supply and delays tissue repair.
Prevention
General prevention advice: Wear seat belt.
Don’t carry objects that are heavy. Use a step stool. Do not stand on chairs or other unsteady tables.
Wear knee guards during sports or recreational activities, such as roller-skating or soccer or cycling.
Stretch before and after physical exercise, sports, or recreational activities to warm up and wake your muscles, do not strain them.
Use equipment appropriate to your size, strength, and ability. Avoid repeated movements Have a trainer or person who is familiar with sports equipment to check your equipment to see if it is well suited for your level of ability and body strength.
If you feel that certain activities at your workplace are causing pain from overuse, find other ways of doing your job or to talk about using different equipment.
Keep your knees and the muscles that support them strong and flexible… Try the following stretches: Hamstring stretch, Knee-to-chest exercise, Calf stretch and Straight-leg raises
Avoid activities that stress your knees as deep knee bends or downhill running.
Wear appropriate shoes with good arch supports.
Do not wear high-heeled shoes.
Replace running shoes every 400 to 600 miles kilometers.
Prolotherapy
Aging Knees regeneration and repair of damaged ligaments and support structures of the knee are proved to be successful in USA with Prolotherapy.
Dr Kapil Bakshi is a USA trained Prolotherapy expert. The second surgeon in UAE to have undertaken this training.
Prolotherapy provides Non-Surgical Management of Knee Osteoarthritis in patients not opting for surgery or who are unfit for surgery.
SAVE CARTILAGE from AGING – STRESS – INJURY
- Stop Enzymatic (Collagenase) Degradation of Cartilage
- Chondral (Cartilage) Protection via Inhibition of Cox -2 expression
- Reduce production of Wear and Tear Pro-inflammatory Cytokines (TNF-a /IL-1 IL-6)
- Deactivate Killer T-cells mediated inflammatory process
References from most advanced research published highest impact factor journals
PRP Improves Clinical Outcomes in Chronic Tennis Elbow Mishra
PRP References AJSM 10; PRP vs steriod injection for lat Epi Peerbooms
PRP in UCL tears of the elbow Podesta
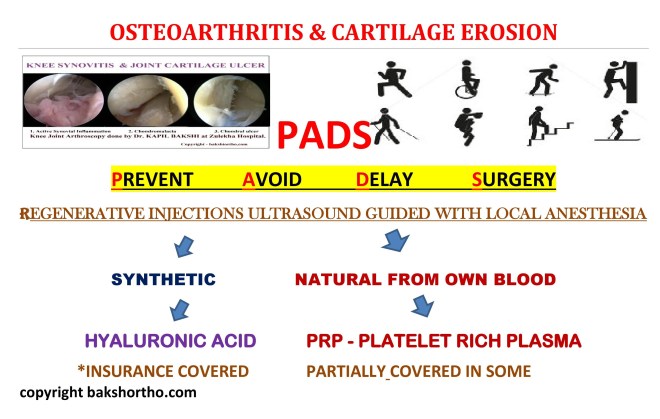
Cartilage Erosion with age and overuse
Causes of Chondromalacia Patella:
* Anatomical or Mechanical Variations: Q-angle: The most important cause of Chondromalacia patella is abnormal Q-angle. Normal Q-angle for men is 14◦ and for women, it is 17◦. The lateral pull of the patella is increased if this angle is increased which then can lead to Chondromalacia patella.
* Muscle tightness: If the rectus femoris muscle is stiff due to spasm, it affects the patellar movement when the knee is bent. Iliotibial band muscle tightness with tight lateral retinaculum pulls the patella to the lateral side of the knee when the knee is bent.
* Trauma: Knee instability caused by a previous cruciate ligament or meniscal deficiency, trauma or misuse of the knee can lead to Chondromalacia patella. Repetitive trauma and inflammatory conditions like arthritis can increase the incidence of chondromalacia.
-
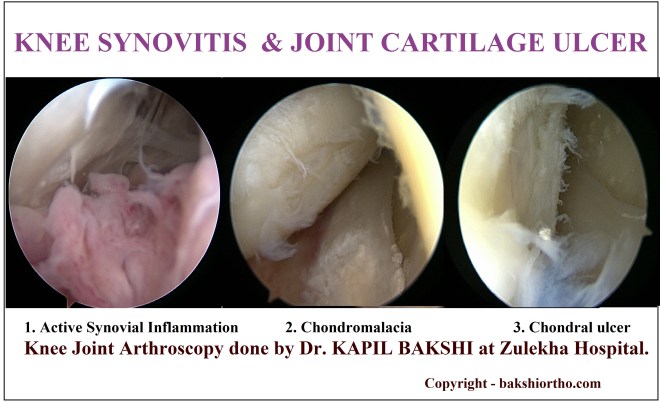
‘Chondromalacia Grades “Bakshi” on Ultrasound’ and Arthroscopy (Author: Dr. Kapil Bakshi)
* grade I :
arthroscopically: softening or swelling of cartilage
* grade II
* blister-like swelling/ multiple hyper intense streaks in parallel to the bone surface suggesting fragmentation and fissuring within soft areas of articular cartilage
* grade III
* arthroscopically: partial thickness cartilage loss with fibrillation (crab-meat appearance)
* grade IV
* arthroscopically: cartilage destruction with exposed subchondral bone
CARTILAGE MAPPING ON MRI 
ARTHROSCOPY
Swollen Knee With Traumatic Hemarthrosis and Inflammatory Synovitis
Platelet Rich Plasma Biology
Growth Factors
Due to relative avascularity, tendons may lack adequate
growth factors for healing
PRP contains Growth Factors
○ Platelet Derived Growth Factor
Chemoattractant for WBCs, macrophages, stem cells
○ Transforming Growth Factor-beta
Promotes cell proliferation
Increases Type 1 collagen synthesis in tendon
○ Vascular Endothelial Growth Factor
Angiogenesis
○ Basic Fibroblast Growth Factor, Connective Tissue Growth Factor,
○ Epidermal Growth Factor, Insulin Like Growth Factor-1
○ Many other bio-active factors





BONE MARROW ASPIRATE CONCENTRATE
Bone marrow aspirate from iliac crest or tibia is then concentrated and can be used as stem cell therapy for injection into the joints for regeneration of cartilage. This would soon be a reality.
USEFUL LINKS
Knee pain prevention tip
Injury Prevention
http://newsroom.aaos.org/patient-resources/prevent-injuries-america/
Dr. Kapil Bakshi. M.S (Master of Surgery)
Professional Orthopaedic Surgeon (MOH Specialist ‘A’ Orthopaedics)
Right Medical Center, Sharjah, UAE









